
Eye Care
Exceptional eye care since 1958
Services
At Osmond Drake, we are committed to providing the highest standards of care and professionalism from the first moment you enter our practice.
We’ll carry out a thorough investigation of your eyes, including a vision check, spectacle prescription, ocular health examination plus any other tests that you may require; all while catering our services to your unique needs and lifestyle.
Once we’re satisfied with your prescription and eye health, and have taken the time to understand your needs in more detail, we’ll make recommendations based on your individual circumstances. We will explain our findings to you clearly simply, and can always provide further information if needed.
Rest assured, all examinations and treatments are undertaken using the very latest ophthalmic technology by our highly trained staff. We are dedicated to maintaining exceptional levels of clinical care and customer service.
Some patients will not require an Enhanced Eye Examination. If you’re under 40 and have no known eye conditions and no health concerns, our Standard Eye Examination will be adequate.
What happens in a sight test?
The sight test is made up of several parts which come together to ensure we perform a thorough check of your eyes. Don’t worry – your optometrist will guide you through every part of the sight test.
- First, your optician will ask you some questions about any problems you’ve been having with your vision or your eyes; including blurriness, discomfort, discharge and so on. They will also ask about any problems you’ve had with your eyes previously, your general health, medications, whether you drive, and your occupation. This lets us tailor the eye examination to your individual needs, making sure we provide you with the best check possible.
- Next, they will check your vision by asking you to read off the chart. They will show you some different lenses to work out the best spectacle prescription for you.
- Then, your optometrist will use a microscope to examine your eyes and check for any ocular health issues.
- Finally, the optometrist will explain their findings and make some recommendations on how you can make the most of your vision and keep your eyes healthy. This may include getting new glasses, contact lenses, suggesting lifestyle changes that will help you keep your eyes healthy, safety glasses, sports goggles, or alternative options to keep your eyes at their best.
There are some other tests your optometrist may perform to help them check your eye health. These may include:
- Eye pressure check. Don’t worry – we don’t do the air puff test any more! This test is painless and quick, and lets us check the pressure in the eye is healthy.
- Visual fields test. This lets your optometrist make sure that your peripheral vision is as it should be.
- Colour vision test. These checks allow your optometrist to tell if you see colours in the same way as most of the population. This is important for certain jobs, eg. train drivers and electricians.
- Topography. This is when your optometrist measures the curvature of the surface of your eye.
If you have any questions about any of the tests, please ask one of our friendly staff members.
This can be covered by the NHS (if eligible) or privately at a cost of £35.
Enhanced Eye Examiations cover everything required for a sight test, plus an OCT scan of the inside of your eyes.
OCT scans allow us to investigate the eye health in more detail, and provide a lasting record of the eye health. We can then compare them to any scans taken in the future, allowing us to pick up on changes to your ocular wellbeing sooner than otherwise.
Enhanced Eye Exams also last longer, giving more time with the optometrist for in depth advice and to answer any questions you may have.
What happens in a sight test?
The sight test is made up of several parts which come together to ensure we perform a thorough check of your eyes. Don’t worry – your optometrist will guide you through every part of the sight test.
- First, your optician will ask you some questions about any problems you’ve been having with your vision or your eyes; including blurriness, discomfort, discharge and so on. They will also ask about any problems you’ve had with your eyes previously, your general health, medications, whether you drive, and your occupation. This lets us tailor the eye examination to your individual needs, making sure we provide you with the best check possible.
- Next, they will check your vision by asking you to read off the chart. They will show you some different lenses to work out the best spectacle prescription for you.
- Then, your optometrist will use a microscope to examine your eyes and check for any ocular health issues.
- Finally, the optometrist will explain their findings and make some recommendations on how you can make the most of your vision and keep your eyes healthy. This may include getting new glasses, contact lenses, suggesting lifestyle changes that will help you keep your eyes healthy, safety glasses, sports goggles, or alternative options to keep your eyes at their best.
There are some other tests your optometrist may perform to help them check your eye health. These may include:
- Eye pressure check. Don’t worry – we don’t do the air puff test any more! This test is painless and quick, and lets us check the pressure in the eye is healthy.
- Visual fields test. This lets your optometrist make sure that your peripheral vision is as it should be.
- Colour vision test. These checks allow your optometrist to tell if you see colours in the same way as most of the population. This is important for certain jobs, eg. train drivers and electricians.
- Topography. This is when your optometrist measures the curvature of the surface of your eye.
If you have any questions about any of the tests, please ask one of our friendly staff members.
This examination costs £55 privately or £30 for NHS patients.
Optometrists with an Independent Prescribing (IP) Qualification are able to provide emergency eye care where they can assess a patient, establish a diagnosis, determine the clinical management required and prescribe where necessary.
During COVID lockdown, Marc was one of four practitioners chosen to help support the NHS Cardiff & Vale Trust which the practice continues to this day.
You could have an acute eye condition if you have any of the symptoms below.
- Sudden blurred / loss of vision
- Sudden onset flashing lights in your vision
- Sudden onset floaters in your vision
- Sudden onset headache
- Eye pain
- Red eye
- Halos around lights
- Other sudden changes to your eyes / vision that cause concern.
Contact us for advice. We will triage your symptoms and offer you the appropriate care.
This maybe a routine eye examination, or if required, an Eye Health Examination Wales (EHEW) check within a suitable time frame.
If we are not able to offer an examination promptly, we will arrange for an EHEW at another practice nearby.
You can refer yourself for EHEW and also be referred for EHEW by your GP or other health professional such as a practice nurse or pharmacist.
At the EHEW your eyes will be examined and your optometrist will diagnose the problem and decide whether they can treat your symptoms, or if you will need to be referred to an IP-qualified optometrist or to the hospital’s Ophthalmology Department.
Eye Health Examination Wales checks are NHS-funded tests to allow patients requiring advanced services to access them easily and in a timely manner.
Patients eligible for EHEW tests are those experiencing eye problems that have come on in the last week, or patients at risk of sight-threatening conditions due to health issues, family history or genetic background.
The aim of EHEW is to pick up any eye problems quickly and have them treated as soon as possible.
Please see http://www.eyecare.wales.nhs.uk/eye-health-examination-wales for more information.
If you feel you require an EHEW examination, please contact us to speak to one of our colleagues who will be happy to advise you.
Some optometrists (including Marc Drake and Hannah Jones who work here at Osmond Drake Opticians) have done an extra qualification, known as the Independent Prescriber Course, which allows them to prescribe medications for eye problems. This means that we can treat some issues in practice that used to have to be treated in the hospital.
Independent Prescribers (IP) can accept referrals from other opticians, but you must be seen by your usual optician first so that they can diagnose the problem and refer you on to an IP-qualified optometrist.
You could have an acute eye issues may cause symptoms like:
- Sudden blurred / loss of vision
- Sudden onset flashing lights in your vision
- Sudden onset floaters in your vision
- Sudden onset intense headache
- Eye pain
- Red eye
- Halos around lights
- Other sudden changes to your eyes / vision that cause concern.
Contact your usual Optometrist Practice for advice. They will offer you an Eye Health Examination Wales (EHEW) or arrange for an EHEW at another practice nearby.
You can also be referred for EHEW by your GP or other health professional such as practice nurse or pharmacist.
At the EHEW your eyes will be examined and your optometrist will decide if they can treat your symptoms themselves, or if you need to be referred on to either an IP-qualified optometrist or to the hospital.
The IPOS practice on the rota will try to see the patient promptly.
Further information on EHEW can be found at http://www.eyecare.wales.nhs.uk/ehew
This includes a search function to find your nearest practice. http://www.eyecare.wales.nhs.uk/search-for-services-in-your-area
There are currently 19 in The Vale of Glamorgan, 42 in Cardiff, and around 340 in Wales as a whole.
You must be resident in Cardiff & Vale to access IPOS.
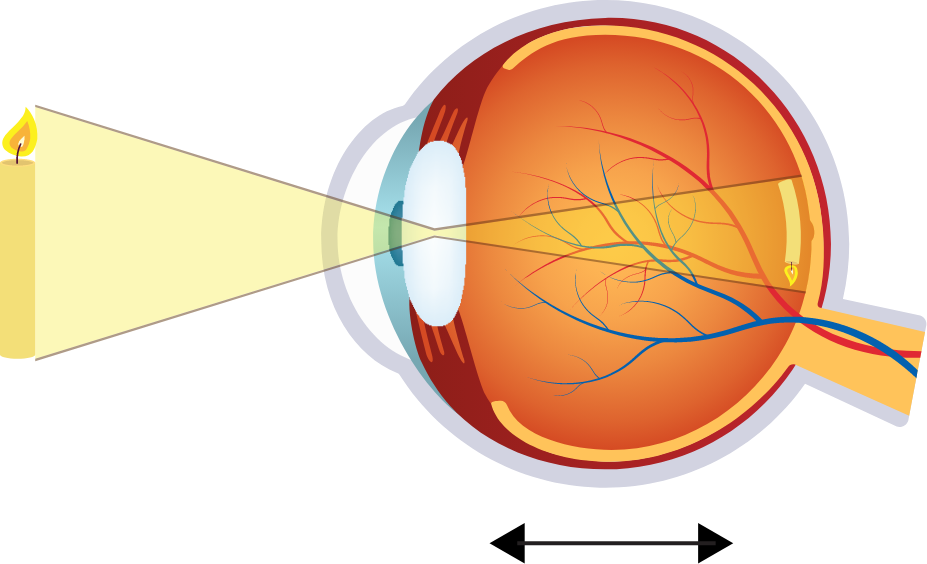
Ocular Coherence Topography (OCT) is an advanced eye scan for people of all ages. It is similar to ultrasound, but it uses light rather than sound waves to map the different layers that make up the back of the eye.
We also capture a digital photograph of the surface of your eye to cross- reference any areas of concern. The scan is non-invasive, painless, and only takes a few seconds. It can automatically detect subtle changes to the retina with every test you have done.
OCT stands for Optical Coherence Tomography.
This machine scans the inside of the eye, providing highly detailed images of your internal ocular structures. This allows a more accurate and in-depth examination of the ocular health, aiding in diagnosis and management of any ocular issues. It also provides peace of mind for yourself as you know a thorough check has been made.
The OCT scanning is included in our Enhanced Eye Exams and your Optometrist will show your scans to you and explain the results.
Contact us to book and Enhanced Eye Examination today!
OCT scans are an excellent tool that can be used to detect and monitor many eye complaints.
OCT allows us to see individual layers of the eyes which are not otherwise visible, allowing us a more in-depth examination of your ocular health. Some eye problems can be found sooner with OCT than they can without it, allowing for quicker diagnosis and treatment.
Examples of ocular issues that can be detected with OCT are:
- Age related Macular Degeneration (AMD)
- Diabetes
- Glaucoma
- Macular Holes
- Vitreous detachments
If you are under the care of a private consultant, they may request that you attend our practice for OCT scans.
We are happy to provide this service, though you will need an appointment for your scans to be taken.
The cost of the scans will be £40-£60, depending on which scans are needed and whether your Optometrist needs to review the data first.
OCT scans are included in our Enhanced Eye Examinations and for Iris members.
Here are some frequently asked questions about our eye care.
If your question isn’t answered here, please feel free to call the practice with any queries you may have.
We usually begin testing children at four years old. However, if you suspect that there is a vision issue with your child at any point, please contact us to arrange an appointment and we will be happy to check.
Sight tests are important even if you do not notice any eye or vision problems. This is because children cannot always tell if their vision is blurred and so it’s key that they have an examination to ensure that they are seeing normally.
Symptoms indicative of problems include:
- Rubbing of eyes
- Squinting
- Turning or tilting their head
- Losing their place or using a finger to follow the line when reading
- Moving their head or mouthing words whilst reading
- Headaches
- Red eyes
- Wandering eyes
- Complaints of blurred vision.
We suggest yearly checks for people who are under sixteen years old, as the eyes can develop and change as children grow.
For people who are sixteen to sixty-nine years old, we recommend sight tests once every two years.
People seventy and over usually have sight tests once a year due to the increased risk of ocular problems as time goes on.
If you have Diabetes, yearly tests are best to check for any diabetic changes to your eyes, no matter what age you currently are.
If you are over forty and have an immediate family member (parent or sibling) with glaucoma, we prefer to check once a year as there is a lightly higher chance that glaucoma may develop.
If you start to suffer from headaches, double vision, blurred vision or any other abnormality in your vision, book an eye examination straight away.
You do not need to see your doctor before having an eye test, though your doctor may refer you to us if they feel it is necessary. All you need to do is make an appointment by calling 029 20709526.
You are entitled to an NHS Eye Examination if:
- You are under 16 years of age
- You are under 19 years of age and in full time education
- You are 60 or over
- You or your partner receive Universal Credit, Income Support, Income Based Jobseekers Allowance, Income Related Employment and Support Allowance, Pension Credit, or Tax Credit.
- You are named on a valid HC2W Certificate
- You are registered severely sight impaired
- You suffer from diabetes or glaucoma
- You are considered at risk of glaucoma by an ophthalmologist
- You are 40 years over and are the parent/sibling/child of a person with glaucoma
- You are a prisoner on leave from prison
- You have been prescribed complex lenses under the NHS optical voucher scheme.
Cataracts are caused when the lens inside the eye clouds over to become misty. This happens to everyone over time, usually from the 60s onwards.
It can be brought on earlier in some circumstances, for example following trauma or surgery, in people with diabetes, or if there is a family history of cataracts developing early.
Early cataracts can be managed with glasses and/or contact lenses. If they progress enough, however, they will require cataract surgery.
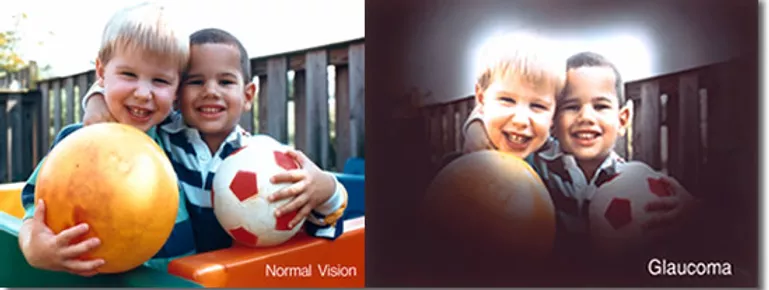
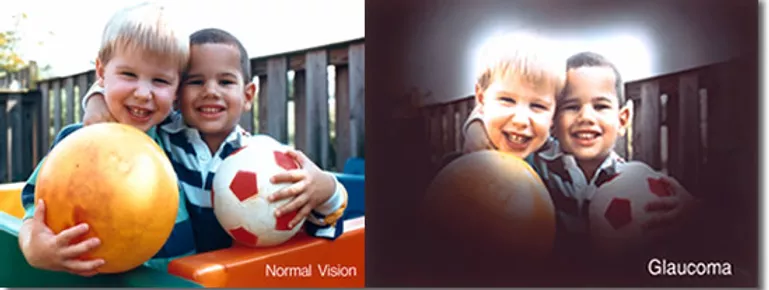
Glaucoma is a type of ocular issue where the optic nerve, which relays information from the eye to the brain, becomes damaged. This causes vision loss in the peripheral vision, which can eventually cause missing patches in your sight or tunnel vision.
What causes glaucoma?
Glaucoma is caused by either high pressure in the eye, or because the eye is more susceptible to damage from high pressure in the eyes.
What are the symptoms?
Most kinds of glaucoma do not show any symptoms at all until it is very advanced. This is why it is important to have regular sight tests, especially if you have an immediate family member (parent or sibling) with glaucoma.
Rarely, glaucoma can cause symptoms of red, painful eyes with blurred vision, haloes around lights and nausea. If you experience these symptoms, please contact your optometrist immediately.
What are the treatments?
Glaucoma is usually treated with drops which bring down the pressure within the eye. If these are not successful in stopping the progression of the glaucoma, your consultant may consider other options, such as laser or surgery, though this is rare.
It is rare for people to lose their vision due to glaucoma, as long as it is diagnosed and treated.
Age-related Macular degeneration, or AMD, is the biggest cause of sight loss in the UK.
It is caused by age changes at the back of the eye, affecting the macula, which is the most sensitive part of the retina that makes up the central part of your vision. These age changes can alter the vision in a number of ways, most commonly causing distortion in the vision.
What can cause AMD?
Age-related macular degeneration can run in families. It is recommended that you have regular sight tests if you have a parent or grandparent with AMD. We suggest our Enhanced Eye Examination, as OCT scans are included in this test. This allows us to have a more thorough and in depth check of the macula and other ocular structures.
Lifestyle can also affect your chances of developing Macular Degeneration. People who smoke are up to four times more likely to develop AMD than people who do not. Sun damage to the eyes also makes AMD more likely.
How can I avoid developing AMD?
The best ways to avoid AMD are:
- Not smoking and avoiding second hand smoke
- Protecting your eyes from the sun with sunglasses and a brimmed sunhat
- Eating a varied diet with lots of brightly coloured and green leafy fruits and vegetables.
Presbyopia, or the need for reading glasses, is a normal and natural process – though it can be very annoying!
The lens inside the eye is flexible in childhood. This means that it can change its shape, altering the focus so that you can see near tasks like books and phone screens.
This lens is the only part of your body which never stops growing. Due to this, the lens becomes more and more dense over time. It eventually becomes so dense that it can no longer change its shape to focus close tasks – this is when you begin to need reading glasses.
People usually begin to struggle with reading when they are between 40-45 years old. This may be earlier if you are long sighted, or later if you are short sighted. It gradually worsens over time, and you will need to update your prescription every two years or so, until things stabilise at around 70 years of age.
If you have any trouble with your vision, please contact us to arrange an appointment.
Both Bifocals and Varifocals allow you to see more than one distance. This is different to distance and reading glasses, which only focus one distance.
Bifocals
Bifocals focus two distances – far away from you, eg. road signs and television; and near, eg. books and magazines.
Bifocals have a line across the lower part of the lens. Above the line, the lens focuses the distance vision. Below the line, the prescription is designed to help you see close work.
This line is visible to other people, so they can see that you are wearing a bifocal lens. Some people also find it strange having a sudden change within the lens, from distance to near. However, most people get on well with bifocals.

Varifocals
Varifocals focus many distances, including distance, intermediate (eg. computer distance) and close.
Varifocals do not have a line on the lens; instead, the lens changes strength gradually. The lens is designed so that you can see the distance when you are looking straight ahead, you can see intermediate distance slightly below this, and the reading portion of the lens is slightly lower still.
Varifocals do take some getting used to. However, most people find them convenient and easy to use.

If you would like to try Bifocal or Varifocal lenses, please contact us on the number at the bottom of this page!
Eye Conditions
Regular eye examinations are important for everyone, as some serious eye conditions do not have any visible warning symptoms.
It’s especially important to have regular check ups if there is a history of eye conditions in your family.
Blepharitis is a condition in which chronic inflammation of the eyelid margins causes symptoms of eye irritation, feeling of dryness, red rimmed eyelids and watering. Sometimes there are no symptoms.
There are two types of blepharitis, which sometimes occur together:
- Anterior blepharitis – which affects the outside front edge of the eyelids (on and around the roots of the eyelashes)
- Posterior blepharitis – which is also called Meibomian Gland Dysfunction (MGD), results when the condition affects the inside rims of the eyelids (just behind the eyelashes) which contain the meibomian glands. The meibomian glands produce a thin layer of oil which normally prevents the tears from evaporating too quickly; if they are inflamed, this mechanism does not work properly.
Hot compresses, either in the form of an EyeBag or a hot towel, can be used to help treat Blepharitis. Lie down and place the hot compress over your closed eyes. Leave it there for ten minutes to allow the heat to soak in to the eyelids.
Following this, use eyelid cleaning products (available at Osmond Drake Opticians) or cool boiled water to clean the eyelids and remove anything that may be irritating the eyes.
More information on these techniques can be found on our Dry Eye page by clicking here.
Antibiotics in the form of eye drops or ointments (and in some cases antibiotics taken by mouth) can potentially lessen symptoms and are effective in clearing bacteria from the eyelid margins in extreme cases.
These treatments help to keep the symptoms of Blepharitis under control. However, they do not cure the issue – you must keep doing the treatment regularly or the symptoms will come back.
If you suffer from blepharitis, we recommend that you join our Iris Membership Scheme so that we can monitor you regularly. You will also receive discounts on any products purchased to treat this condition.
A cataract forms when the lens inside the eye, which helps to focus the light, becomes gradually more hazy. This means that less light can enter the eye and the vision seems more blurred.
Cataracts can affect either one or both of the eyes.
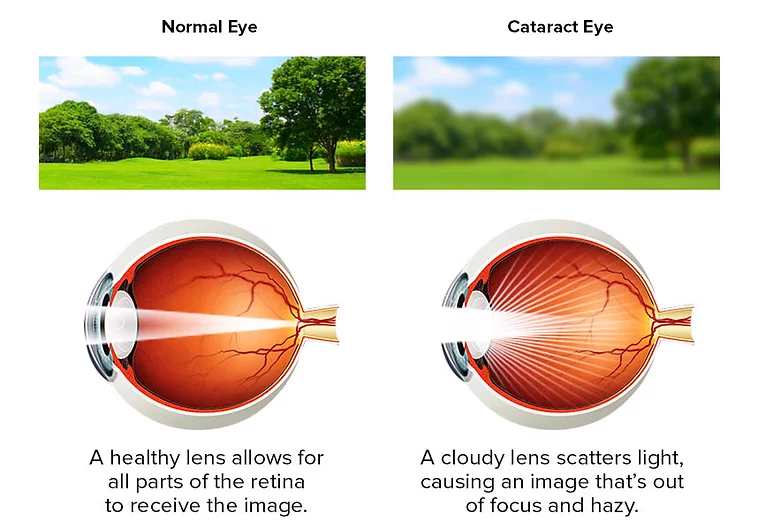
Cataracts are usually associated with increasing age, but they can also be caused by medications, other eye conditions, or trauma to the eye.
Symptoms
Early cataract: possibly none, or mild blur that can be helped with glasses.
More advanced cataract: increasing blurred vision, colours looking different (eg. whites can look cream), glare (eg. from headlights when driving in the dark), trouble seeing at night, needing more light to read, and on rare occasions double vision.
Developing cataracts can also make you more short-sighted.
Diagnosis
If you notice any of the above symptoms, please contact us to arrange an appointment with one of our optometrists. If cataract is the cause, they will see this during the test and discuss your options with you.
Treatment
If treatment is required then you will need a short operation. Surgery is performed through a tiny hole in the eye and your own lens is replaced with a plastic implant.
However, not all cataracts require treatment. If you are not having any problems and your quality of life is not affected, surgery is not usually required.
Most patients are delighted with the results of their cataract surgery, though it can take between three to six weeks to completely recover from the procedure
After surgery, patients say that:
- Things are clearer (once they have their updated vision correction)
- Glare is not as noticeable or as annoying
- Colours seem brighter and more distinct
If you have another condition affecting your eyes, such as macular degeneration, diabetes or glaucoma, you may still have limited vision, even after successful surgery. Your optometrist and ophthalmologist will discuss with you at your appointment.
Cataracts are caused by the lens inside your eye becoming clouded over time. This happens to everyone eventually, though it can happen sooner in people who have diabetes, have been exposed to a lot of UV light, or have had trauma to the eye.
The most common symptom of cataracts is blurred vision. Other common symptoms are: glare from lights at night, eg. while driving when it’s dark; colours looking different (eg. what looks cream to you may seem white to someone else); haloes around lights.
If you notice any of these symptoms, please contact us to arrange an appointment.
If you have cataracts, your optometrist will let you know during your sight test. In the early stages, nothing needs to be done except to have the eyesight and eye health monitored. Eventually, though, the cataract will need to be removed with surgery.
If you require referral, your optometrist will ask you to return on another day for a followup appointment. During that appointment, they will put drops in the eyes which will make your vision blurred – therefore you should not drive to that appointment. At this appointment they will double check their findings and discuss the cataract surgery procedure with you, allowing you time to ask any questions that you might have. Following this appointment, they will refer you to a consultant ophthalmologist for cataract surgery.
You can choose between being referred on the NHS, or privately. The NHS waiting list in Cardiff and Vale Health Board is currently about two years long, though they are working hard to bring this time down. If you would prefer to go privately, you will generally be seen within two months.
At the assessment you will be asked about your vision problems and their effect on your quality of life. The ophthalmologist and their team will examine your eyes and take some measurements of your eye (Biometry) to help them decide which lens would give you the best vision. They will take this into account when selecting the plastic implant lens that will be inserted during the operation. A nurse will go through some relevant health checks and talk you through the procedure and answer any questions you may have.
If surgery is offered and you decide to go ahead, a date will be arranged for surgery.
The surgery will normally take 10-20 minutes. Most cataract operations are performed under a local anaesthetic, so you’ll be awake. Most people say that they can only see a bright light during surgery, while some say that they see a little bit of movement (though nothing specific). Your ophthalmologist and anaesthetist will make sure you don’t feel anything, as well as talking you through everything they’re doing.
Your ophthalmologist will make a very small cut in the eye to remove the cataract and then replace it with an artificial lens. In most cases stitches aren’t needed. After the operation, you’ll initially need to keep your eye covered to protect it from any accidental damage. You can go home the same day, but you won’t be able to drive. Someone will need to look after you for about 24 hours after your procedure.
After cataract surgery, you will be mobile, but you will need to make sure that you rest. It’s normal to experience some itchiness, sticky eyelids, or fluid discharge during this time.
Mild discomfort can be managed by taking paracetamol as advised. After a few days even mild discomfort should begin to disappear, and in most cases, healing will take about two to six weeks.
During recovery you’ll need to wear a plastic shield at night to protect the eye when sleeping. You’ll also need to use eye drops for about four weeks to reduce inflammation and prevent infection.
Your ophthalmologist will discuss all these details with you during your appointment and will advise on the follow-up care they recommend. Unless you are a complex case, this is usually provided by optometrists (like us!) four weeks after your surgery.
Cataracts are caused by the lens inside your eye becoming clouded over time. Cataract surgery involves removing this lens and replacing it with a clear plastic lens.
The consultant who does your surgery will measure your eye and take your prescription into account. This will help them choose what lens to put into your eye, as they will usually try to correct your distance vision with the new lens. This means that you should be able to see well in the distance without glasses (though there is sometimes a small prescription left over). You will still need reading glasses to help with the close work.
Your consultant may offer to leave one or both eyes short sighted after the surgery, especially if you were already short sighted before. This will mean that you can see to read close up without glasses on. However, you will need glasses to sharpen the distance vision.
If you opt to have your cataract surgery done privately, you can have a varifocal-style lens used to replace your cataract. These lenses help you to focus both at near and distance, meaning that ideally people do not to wear glasses after having these lenses (though some people do find their vision is a little better with glasses still). These lenses can cause a halo effect around lights, especially in the dark. There is usually an additional cost for these lenses.
You should always have a sight test about four weeks after your cataract surgery so that your vision can be checked and you can be provided with glasses if necessary.
If you have any queries, please get in touch.
Cataract surgery is extremely common, with millions of patients having it done every year. Most surgeries are successful, though there is always a slight risk of infection or other complications.
The risk of complications is estimated at around 1 in 50 cases. These can include: blurred vision, some loss of vision, detached retina – where the thin layer at the back of your eye (retina) becomes loose.
Most of these serious complications can be treated with medicines, laser treatment or further surgery.
There is a very small risk (around 1 in 1,000) of permanent sight loss in the treated eye as a direct result of the operation.
These risks will be discussed with you by your optometrist before you are referred to an ophthalmologist. They will be discussed again in the Eye Clinic and you will be asked to give consent for surgery.
What is Glaucoma?
Glaucoma is caused by damage to the Optic Nerve (the nerve that relays information from the eyes to the brain). If left untreated, glaucoma can eventually lead to blindness, but this is very rare in this day and age.
Glaucoma is usually picked up in a sight test, as there are not usually any symptoms. In advanced cases, patients may eventually find that they start to lose the edges of their vision, giving the effect of looking through a tunnel. Left untreated it would eventually lead to complete loss of vision.
What Causes Glaucoma?
Not everything is known about the causes of glaucoma.
We do know that it is sometimes caused by high pressure in the eye. This can happen if the eye’s drainage system becomes blocked; either due to age, injury, or a number of other reasons. This can lead to the pressure building inside the eye and this in turn can damage the optic nerve.
Because there are usually no early symptoms it is important to have regular checks. This is particularly important for people who are over 60 years old, or if there is a family history of the condition as glaucoma does tend to run in families.
What is the treatment?
Glaucoma cannot be cured, but treatment can be used to try to prevent it from worsening. Most glaucoma patients are treated with eye drops to keep the eye pressure low. If this does not work, sometimes laser procedures or surgery is used to help the eye fluid to drain more easily.
If you have any questions, please call us to arrange an appointment to speak to one of our optometrists.
Advanced procedures available at Osmond Drake, such as OCT Scanning, are part of our Enhanced Eye Examination.
What is Keratoconus?
Keratoconus occurs when the clear part on the front of the eye, or cornea, becomes misshapen. This causes changes to the prescription as the eye will become more short sighted and the astigmatism will increase, meaning that the vision will become more distorted. Sometimes this becomes bad enough that the vision cannot be fully corrected with glasses, meaning that contact lenses or other methods are required to improve clarity.
What are the symptoms?
Common symptoms of Keratoconus include:
- Blurred Vision
- Increasing Myopia
- Increasing Astigmatism
- Distorted Vision
- Glare
- Halos around bright lights
- Poor vision not correctable with glasses or soft contact lenses
What are the causes?
The cause of Keratoconus is unknown. It usually arises in the teenage years and stabilises in the early twenties.
There are probably several genetic components as approximately 5% of cases run in families. It is also more common in people with significant allergy or “atopy,” such as eczema and asthma.
Some atopic patients with Keratoconus have a history of eye rubbing which is known to cause worsening of keratoconus through microscopic corneal trauma.
What treatments are available?
Modern treatment for Keratoconus are designed to stabilise the condition and improve the vision.
Current treatments include:
- Specialist Contact Lenses
- Corneal Collagen Cross Linking (CXL)
- Intra-Stromal Rings
- Topography Guided PTK combined with CXL
- Implantable Contact Lenses
- Corneal Transplantation
The retina is the skin inside the eye that contains the photoreceptor cells, which react to light. The most sensitive part of the retina is the macula. This is because more photoreceptors live in the macula than anywhere else in the retina, allowing the macula to see more fine detail.
Age Related Macular Degeneration, otherwise known as AMD, affects the macula. It is caused by age changes over time damaging the retina and therefore making the vision worse. AMD is the leading cause of vision loss in the UK.
Macular Degeneration comes in two forms: Dry AMD and Wet AMD. Dry AMD tends to affect the vision less, though there is no treatment currently. Wet AMD can be treated with injections to try to stop it from worsening and tends to have a larger impact on the vision.
AMD can run in families and those with a parent or grandparent that has it have a higher chance of having the condition themselves at some stage. However, there are many lifestyle factors that can make it much more likely that a person will develop AMD. These lifestyle factors are:
- Smoking. People who smoke are up to four times more likely to develop AMD.
- UV light damage
- Poor diet.
Stopping smoking, protecting your eyes from the sun by using brimmed hats and sunglasses with a UV filter, and a varied diet with lots of brightly coloured fruits and vegetables are the best ways to prevent AMD.
Changes to your diet and lifestyle can help protect you from AMD. Supplements such as I-Caps to help maintain macular health are available in practice. We strongly recommend regular OCT 3D scans if you are concerned about AMD.
Presbyopia is a natural part of ageing and something that most of us will experience at some point in our lives. You will notice that things begin to get blurry at normal reading distance. You may find that you start stretching your arm out to hold things further away when you’re trying to read. You may also get eye strain or headaches. This is frustrating, but is natural.
What causes presbyopia?
The lens inside your eye helps to focus the light. In childhood, this lens is flexible and can change its shape to focus things close to you. This lens is the only part of your body that never stops growing. It gradually becomes more and more dense until it can no longer change its shape. When this happens, you begin to notice that things close to you are no longer clear.
Solutions for Presbyopia
Unfortunately, there’s no way to stop or reverse presbyopia.
However, you can still see well at close distances with either glasses or contact lenses. At Osmond Drake, we can help you find a solution that suits you.
Your options include:
- Reading glasses
- Varifocal glasses
- Bifocal glasses
- Monovision contact lenses
- Multifocal contact lenses
Whichever option you choose, it’s important to remember that presbyopia will change over time.
So, it’s important to keep up-to-date with your eye examinations so that your prescription is always accurate.
Eye Health
Are you eating the foods that are best for your eyes?
Your diet is extremely important in maintaining eye health.
We’ve all heard that carrots are good for your eyes – but did you know that it’s true? Carrots have lots of beta-carotene, which is vital to eye health.
However, carrots aren’t the only food that’s good for the eyes…

Fish
Fish such as tuna, salmon and mackerel are full of Omega 3 fatty acids which help to protect against dry eye, macular degeneration and even cataracts.

Eggs
The vitamins and minerals in eggs such as lutein and vitamin A, can protect from night blindness and dry eyes, serving to promote eye health and function.

Leafy Greens
Leafy greens such as spinach, kale and spring greens are filled with lutein and zeaxanthin that can help stem the development of macular degeneration and cataracts.

Whole Grains
The vitamin E, zinc and niacin found in whole grains can promote overall eye health. Swapping refined carbohydrates like white bread for whole grain alternatives is an easy way to include them in your diet.

Citrus Fruits & Berries
Oranges, grapefruits, lemons and berries are high in vitamin C which can help reduce the risk of macular degeneration and cataracts.

Nuts
The Vitamin E, Zinc & Niacin found in whole grains can promote overall eye health. Why not try swapping refined carbohydrates for whole grain alternatives for an easy way to add them into your diet?

Legumes
Legumes such as kidney beans, black eyed peas and lentils are sources of bioflavonoids and zinc which can help protect the retina and reduce the risk of macular degeneration and cataracts.

Super Supplements
Supplements such as fish oil, flaxseed oil and blackcurrant oil contain Omega 3 fatty acids which help prevent dry eye syndrome, macular degeneration & cataracts.
Low Vision Appointments
We also offer Low Vision Appointments. You can find out more about this by clicking here.
General Health
Your health in general can also affect your eyes. Things like smoking, poor diet and lack of physical activity can make it more likely that eye problems will develop.
If you would like further information on health, or help changing your lifestyle, please click on the links below.
Healthy Eating and Physical Activity
“We would like to thank you most sincerely for the fantastic professional care and attention you give to our eyes. It’s beyond the call of duty. It cannot be bettered anywhere in the world—and we travelled a great deal of it during our working years. The Drake team is UNBEATABLE!”
M&J Peirson
“Brilliant staff, excellent with children.
Always go out of their way to help.”
K. Porter


We are committed to providing the best care possible which is why all of our staff are trained
to understand the needs of people with Dementia or Autism.eue
If you or a member of your family has been diagnosed with dementia or autism then please
be sure to let our staff know when booking an appointment



